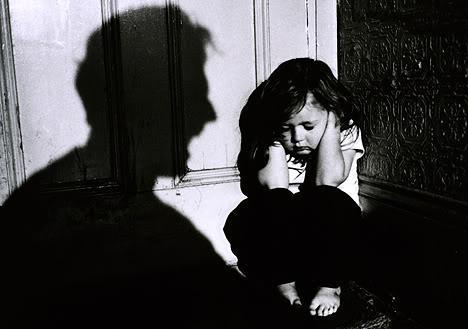
Painful experiences early in life can alter the brain in lasting ways.
A difficult reality for psychiatrists and counselors of child abuse is that young victims are at high risk of becoming offenders themselves one day, although it’s unclear why. But now a team of behavioral geneticists in Switzerland report a possible reason: early psychological trauma may actually cause lasting changes in the brain that promote aggressive behavior in adulthood.
Writing this week Translational Psychiatry, the researchers describe a series or experiments conducted in rats that led them to that conclusion. Animals placed in traumatic, fear-inducing situations around the time of puberty show high and sustained levels of aggression later in life. And while rats cannot substitute for humans, the scared rats also showed changes in hormone levels, brain activity, and genetic expression that appear very similar to traits observed among troubled and unusually violent people.
The main implication of the research, says study co-author Carmen Sandi, is that it links two previously observed phenomena: the higher rate of aggression among those experiencing early-life stress, and the blunted activation of a brain region known as the orbitofrontal cortex among people with pathological aggression. Social learning, it seems, may not be the only thing that makes abused kids more likely to grow up aggressive.
“This is a key finding which highlights the importance of not only developing social programs and politics, but also of reinforcing research that could offer valid [medical] treatments for individuals that have been victimized early in life,” says Sandi, the director of the Brain Mind Institute at Ecole Polytechnique Fédérale de Lausanne, in an email discussing the study. “We need to understand the neurobiological mechanisms to offer better solutions to break ‘the cycle of violence.’”
In the study, Sandi and colleagues tested the rats for changes in specific regions of the brain following long periods of fear, and then tested a potential treatment to determine if it was possible to undo those brain changes.
They began by exposing about 40 pubescent male rats for a few minutes at a time over several days, to severe stress — which, for the rats was either the scent of a fox or being stranded on a brightly lit platform. Those rats immediately showed higher levels of stress hormones and later puberty onset than similar animals not exposed to those experiences.
As adults, the stressed rats showed greater aggression toward other males they met — even ones that were clearly not a threat because they were much smaller or even anesthetized. And the once-stressed animals also showed more signs of depression and anxiety, including a reduced interest in food, lower sociability, and a tendency to give up quickly when faced with a challenge.
Those behavioral changes were accompanied by neurobiological changes in the brain as well. Compared to normal rats, the once-fearful ones had higher levels of the hormone testosterone, which is linked to aggression. They also showed more activity in the amygdala, the part of the brain responsible for emotions such as fear and anxiety, and altered connectivity between the amygdala and a region of the brain involved in decision-making. These brain alterations were also correlated with enhanced expression of the gene for an enzyme known as monoamine oxidase A, or MAOA, providing the scientists with a potential way to reverse the effects of the early traumas. Indeed, treating the rats with an MAOA inhibitor helped to restore normal social behavior and reduce aggression in the formerly stressed animals.
It turns out that the MAOA gene is also related to aggressive behavior in people, and certain inherited variants of the gene have also been linked to aggressive tendencies. Because the new study showed that MAOA inhibitors were effective in treating pathological aggression in rats, Sandi says the findings might suggest a similar drug treatment for humans, too, to complement behavioral therapy.
“What we show in our study is that, regardless of the genetic background, exposure to early life trauma can on its own affect the expression levels of this molecule in the brain,” Sandi says. “Our work is novel in many ways, particularly because it provides concrete neurobiological pathways that link early trauma with pathological aggression.”
Why would early traumatic experiences crave permanent changes in the brain? Evolutionarily, such brain changes may have helped us to survive a harsh and cruel environment, by keeping us on edge and ready to confront any possible threats, Sandi says. Today, however, those same changes may do more harm than good, leading some victims of abuse to slip into a vicious cycle, seeing threats where none exist, and overreacting to situations, often with violence. It’s possible that some people may be genetically more sensitive to the changes triggered by painful experiences, and therefore more likely to benefit from treatments that can address those genetic differences. Better understanding of why vicious cycles of violence exist may help researchers to find ways to break them.
Recent Comments